Get full access with a free account
Benefits of the Coloplast® Professional Educational platform
- Get full access to all educational content, events and resources
- Track your progress
- Share content with your collegues
- Share supporting material with your patient
What is a chronic wound?
Any wound that has not healed in 30-days despite best practice intervention is considered a ‘chronic wound’. Wounds that are not expected to heal within 4 – 6 weeks are therefore automatically considered ‘chronic’ regardless of their aetiology (cause). The guidance given here will help you provide an optimal healing environment for all types of chronic wounds. Even non-healable wounds (i.e. inadequate vasculature or palliative wounds) can be managed by following the recommendations in the Wound Care Pathway.
Wound types

A pressure ulcer/pressure injury is localized damage to the skin and underlying soft tissue usually over a bony area or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shear.

A diabetic foot ulcer is caused by infection, ulceration, or destruction of tissues of the foot associated with neuropathy and/or peripheral artery disease in the lower extremity of a person with a history of diabetes mellitus.

A venous leg-ulcer is a full-thickness defect of the skin that persists due to venous disease of the lower leg. Venous ulceration is a chronic condition that is generally considered to result from venous occlusion, incompetent calf muscle pump function or venous valvular failure, giving rise venous hypertension.

A surgical wound is a cut or incision in the skin that is usually made by a scalpel during surgery. They are usually closed with sutures or staples but are sometimes left open to heal by secondary intention.
Keep in mind:
Any acute wound can turn into a chronic wound if proper wound treatment is not followed!
How to assess a chronic wound
When you assess a chronic wound you should always take both patient and wound into account. By taking a ‘holistic approach’ you have a better chance of determining the best way forward.
A ‘holistic’ wound assessment considers a wide range of factors beyond simply the biology of the wound, and requires coordination between you and the other care providers involved.
When conducting your assessment, you should always use a validated assessment tool, such as the Triangle of Wound Assessment, and ensure that everyone on your team is using the same measurement parameters to assess the wound.
Please find a description of the most important parameters your assessment should include on the following pages.
Chronic wounds need to be re-assessed every 4 weeks to evaluate healing progression and determine if significant changes in the patient’s condition occur.
Remember
The wound is on a patient, the patient is in their environment and the environment is part of a health care system.
How to assess your patient:
➔ Determine age, mobility, dexterity, mental capacity and ability of patient to engage in self-care.
➔ Check for current medications and medication history.
➔ Check for co-morbidities, deteriorating or uncontrolled conditions, wound and pressure injury risk history.
➔ Check for clinical history, such as previous surgeries, wounds and diseases, allergies to medications, etc.
➔ Identify life-style risk factors such as: smoking, nutrition (underweight or obesity), sedentory life-styles and alcoholic/substance abuse.
➔ Check for dermatological diseases and complications such as allergies to treatment products.
➔ Identify sociological issues, such as income instability/employment, housing, social network, social isolation, and overall quality of life.
➔ Identify psychological issues, such as depression, anxiety, etc.
➔ Check for current medications and medication history.
➔ Take note of the experienced level of pain (potential treatment must be assessed both at dressing change and during the agreed treatment plan).
How to assess the type and condition of a wound:
➔ Determine the cause of the wound (the wound aetiology).
➔ Understand the wound’s ‘history’, duration and healing progression.
➔ Register the wound’s location and measure its size (depth, length and width).
➔ Identify bio-burden and check for signs of infection.
Assess the wound depth:
➔ Measure the wound depth.
➔ Inspect the wound bed structure and topography.
➔ Check for exudate pooling.

How deep is the wound?

Was the used dressing the most appropriate?

Do you see exudate pooling?
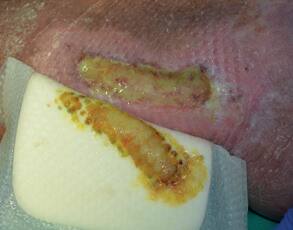
Assess the wound exudate:
- Inspect the used dressing for any leakage (always note when the dressing was last changed).
- Determine the amount of wound exudate in both wound and dressing (how saturated is the dressing?).
- Assess the colour, viscosity and odour of the wound exudate.

Did the previous dressing absorb and retain the exudate?

Is the exudate clear or cloudy?
What colour does the exudate have?
Assess the wound edge and periwound skin:
- Assess the wound edges (are they attached, rolled, inflamed, undermined, advancing, macerated?).
- Assess the periwound skin (is it intact, fragile, inflamed, macerated?).

Is the wound edge and periwound skin macerated?

Is the wound edge undermined?

Are there rolled wound edges?
The Triangle of Wound Assessment
Finally, use a validated assessment tool like the Triangle of Wound Assessment to make your wound assessment.
- Measure and document wound size and depth
- Assess the wound bed
- Assess the wound edge and periwound skin
- Assess for signs of infection using the IWII Continuum and Management Guide
How to develop a treatment and care plan
Once you have completed your holistic patient and wound assessment, an evidence-based treatment plan must be developed. It should define the path forward and be agreed upon by everyone involved - including the patients and their family.
Your treatment plan should focus on:
- Treating the underlying cause/etiology of the wound.
- Managing existing co-morbidities.
- Ensuring effective wound bed preparation and management.
- Selecting appropriate wound dressings.
Treatment Plan - Checklist:
Assess the wound team:
- My treatment plan clarifies who is on the multidisciplinary care team.
- It is accessible and understood by all members of the clinical care team (e.g. physicians, nurses, homecare staff).
- It is understood and agreed to by the patient and the patient’s family/personal support network.
Goal:
- My treatment plan clearly prescribes the care pathway, including specific treatment of the periwound skin and the wound bed.
- It includes specific milestone/targets for the wound’s healing progression (both short-term and long-term).
- It articulates what to do if the targets are not reached.
- It identifies risk factors and adverse events to watch for and instructions on what to do if they arise or are suspected (i.e. early signs of infection, change in wound exudate or wound edge maceration).
Safety:
- My treatment plan makes it clear to the patient when to alert their wound care provider (i.e. warning signs/symptoms of infection).
- It clearly defines when consultation or referral to a specialist is necessary.
How to include the patient and their caregivers
Research shows that patients who are included in planning their treatment and educated on effective self-care are more likely to adhere to their treatment plan.
Including patients and their caregivers means:
- Listening to the patient.
- Working with the patient to find solutions.
- Considering the patient as a partner in care planning.
- Encouraging patient ownership of their own health outcomes.
- Providing tools to help keep patients on track (e.g. providing a copy of the care plan, diaries, progress tracking tools).
- Recognizing and discussing the patient's economic and social realities.
- Accepting the patient’s wishes.
Always keep in mind
A treatment plan should always consider personal preferences and take the patient’s ability to self-care and their personal support-network into account.
Educating patients and their caregivers means:
- Showing them how to perform effective dressing changes.
- Letting them know how to identify signs of infection or other risks that require contact with wound care specialist.
- Providing advice about personal and wound hygiene
- Bringing attention to self-harming behaviours (i.e. smoking, alcohol, hydration, not levating limb or taking off ‘moon boot’).
To help your patients, their family members and care-givers understand, consider using multiple communication methods (e.g. demonstrations, pictures, pamphlets, videos). Also remember to follow up and get confirmation that they have understood.

Always keep in mind
Patient concordance – also referred to as adherence or compliance, is a critical factor in preventing complications and healing chronic wounds. Research shows that engaging patients in planning, including them in decision-making and offering continuous education on effective self-care and prevention is the best way to increase patient concordance.
How to manage a chronic wound
When managing a chronic wound, your main focus should be on preventing complications and creating the optimal environment for wound healing, based on the etiology (cause) of the wound. Based on your holistic assessment you should adhere to the evidence-based standards of care:
- Treat the underlying causes and gain control of co-morbidities
- Manage wound tissue through cleansing and debridement
- Manage wound exudate by managing ‘the gap’
- Prevent or treat infection
How you treat the underlying causes and gain control of co-morbidities will depend on the individual circumstances. In the following pages you will find a guide to managing wound tissue and wound exudate, as well as advice on how to prevent or treat infections.
Cleansing and debridement matters because you are:
- Removing debris and necrotic or non-viable tissue, that provides a medium for bacterial growth, initiates inflammation and delays healing.
- Reducing the inflammatory components and enzymes in the wound.
- Managing the bacterial balance for optimal healing.
Managing wound tissue
How to cleanse:
- Use saline or clean potable water.
- Consider using solutions with a surfactant, antiseptic or antimicrobial agent if infection or biofilm are suspected.
- Cleaning solutions should be at body temperature.
- Apply solution with gentle force to wound bed and periwound skin to loosen superficial devitalized tissue, wound debris, foreign debris and biofilm.
- Aggressive wound cleansing should occur where there is suspected infection or biofilm but this can be painful to the patient and must be managed carefully.

Wound cleansing

Wound cleansing
How to debride:
- Use therapeutic irrigation with a force of 4-15psi (mechanical debridement).
- Debridement pads or wipes can also be used.
- Remove necrotic tissue, slough, debris and biofilm.
- Refashion wound edges to ensure that the skin aligns with the wound bed to facilitate healing.
- Aggressive debridement must be considered when there are signs of infection or biofilm. This can cause considerable pain for the patient.
- Refer to a wound care specialist if aggressive debridement is outside of your scope of practice (conservative sharp, surgical, low frequency ultrasound, chemical andautolytic debridement must be done by a qualified wound care specialist).
- Debriding a wound that does not have adequate vascular supply is not recommended.

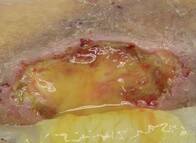
Sharp debridement

Pressure Ulcer before debridement

Pressure Ulcer after debridement
Remember
- Remember: to re-cleanse the wound after debridement with potable water, saline, surfactant, antiseptic or antimicrobial solution.
Managing wound exudate by managing ‘the gap’
After you have effectively prepared the wound bed, it is time to proceed based on your assessment of the wound and wound exudate (See step 1 about assessment). Exudate can be defined as the fluid that leaks from a wound. Wounds produce exudate as a normal part of their healing proces, but an over- or under-production of exudate, or exudate pooling can delay healing and lead to infection. That’s why exudate management is the key to wound healing. You must determine the best dressing choice and frequency of dressing changes to create an optimal moisture balance in the wound.

Low level of wound exudate

Moderate level of wound exudate

High level of wound exudate
To manage exudate you need to:
- Treat the systemic reasons for over or under production of exudate (e.g. inadequate compression therapy for lower extremity wounds, lower limb oedema, nutrition or dehydration).
- Adapt the frequency of dressing changes.
- Choose the appropriate dressing that fill the gap (for more see page 33).
- Educate patient on effective exudate management techniques (compression, elevation, hydration, frequency of dressing changes, etc.).
Always keep in mind
Choose a wound dressing that conforms to the wound bed, manages the exudate and reduces the risk of exudate pooling by fillling the gap between the wound bed and dressing.
Preventing or treating infection
Preventing infection and biofilm should always be a goal of wound care, and effective exudate management is key. But if a wound becomes infected it must be treated. You should check for signs of infection and biofilm at every dressing change.
Warning signs include:
- A healable wound is not healing.
- Changes to the patient’s overall health or wellbeing (fever, etc.).
- Increased amounts of exudate, discoloration, odour.
- Deterioration of wound edge or periwound skin.
- Hyper-granulation – discolouration of the wound bed, granulation tissue, fragile wound bed tissue.
- Biofilm should be suspected if a local infection is nonresponsive to topical antimicrobial treatment.

Local infection

Systemic infection

Suspected biofilm

Suspected biofilm
To effectively prevent or treat infection and biofilm you need to:
- Prepare the wound bed appropriately at every dressing change (cleansing & debridement).
- Apply therapeutic cleansing of the wound and periwound skin, using potable water, saline, surfactant, antiseptic or antimicrobial solution at every dressing change both before and after debridement.
- Debride to remove devitalized or non-viable tissue, bacteria and contaminants.
- Assess wound bioburden at every dressing change using the Wound Infection Continuum (IWII, 2022).
- Manage the wound bioburden.
- Use a dressing with antimicrobial properties for local, spreading or systemic infections.
- Manage exudate by using a dressing that fills the gap between the wound bed and the dressing.
- Change dressings at an adequate frequency.
- Use systemic antibiotics appropriate for the type and level of spreading or systemic infections (avoid prescribing antibiotics when they are not indicated or when their intent is simply to prevent infection or improve wound healing).
- Ensure effective personal and wound hygiene.
- Educate and support the atient to ensure the promotion of a consistently clean environment through hand washing, antiseptic use, etc.
How to choose a dressing
An important part of managing a chronic wound is choosing the appropriate dressing. Whether a dressing is ‘appropriate’ depends on both the status of the wound (is the wound healing? Deteriorating? Infected?) and the frequency of dressing changes you have estimated.
Based on your assessment (see step 1) you have to decide which dressing will best help you manage the wound.
You know you have chosen the appropriate dressing if:
- Its size and shape allows you to secure it to clean dry skin to aid adhesion.
- It removes excess exudate from the wound bed by absorbing and retaining it in the dressing.
- It maintains a moist healing environment.
- It conforms to the wound bed and reduces the risk of exudate pooling by filling the gap between dressing and wound bed.
- It protects the wound edge and periwound skin from trauma and maceration, by vertically absorping the exudate.
- It provides confidence and security to the patient.
- It is comfortable for the patient and makes it easy for the patient to perform self-care in concordance with care regime.
Keep in mind
Consider dressing availability and any socioeconomic constraints or physical/mental limitations faced by the patient.
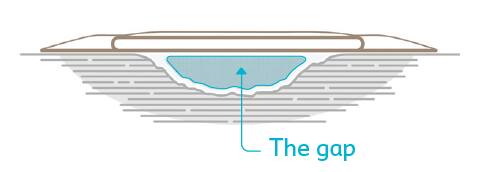
Choose a dressing that conforms to the wound bed and fills ‘the gap’.
Be aware
Always follow locally agreed dressing formularies and local protocols. If a wound is not progressing according to the treatment plan, referral and consultation with a specialist is recommended.

Use a dressing that conforms to the wound bed, absorbs and retains the wound exudate to reduce the risk of leakage and to protect the wound edge and periwound skin.
In case of local infection always consider a dressing with an active component (i.e. silver, honey, iodine, PHMB).
How to monitor patient and wound progression
To evaluate wound progression and check for infections, you should conduct a basic assessment at every dressing change, using an assessment tool, such as the Triangle of Wound Assessment.
The condition of both the wound and patient should match the goals and targets identified in your treatment plan (See step 2 How to develop a treatment plan).
At every 4-6 weeks you should conduct a full re-assessment of the patient and wound - including measuring the wound depth, length and width - to monitor healing progression, overall patient wellness and treatment plan concordance.

Healthy wound edge

Healthy periwound skin

Granulating wound bed

Day 0:
Wound depth 9mm and width 40mm.

Day 40:
Wound depth 2mm and width 25mm.
Keep in mind
You should continue monitoring the wound after skin closure to assess for risks of infection and re-opening.
When you re-assess it is important to determine:
- If the current dressing regime met clinical and patient goals. Remember: The condition of a previous dressing can indicate if change is needed with concern to dressing type or frequency of dressing changes.
- If the treatment plan needs to be changed. Remember: Significant changes in the treatment plan, such as change in dressing type or dressing change frequency, generally requires 14 days of consistent implementation to determine its effectiveness.
- If the patient needs to be referred to a specialist. Remember: A deterioration in the wound or the patient’s overalL well being should trigger automatic referral to a wound care specialist
- If further diagnostics are required.
Glossary
Acute wound
An acute wound is a wound that progresses through the phases of normal healing resulting in closure of the wound, without complications.
Antimicrobial dressing properties
Antimicrobial dressings can be divided into simple and composite dressings. Simple antimicrobial dressings exert only antimicrobial activity, whereas composite dressings exerts, not only the main antimicrobial action also other functions, including exudate normalization, debridement or bioactivity.
Biofilm
Biofilms are microorganisms embedded in a thick, slimy barrier of sugars and proteins that acts as a barrier that shields microorganisms from the patient’s natural immune system and from many antimicrobial agents. Biofilms are a structured community of microbes with genetic diversity and variable gene expression (phenotype) that creates behaviours and defences used to produce unique infections (chronic infection). Biofilms are characterised by significant tolerance to antibiotics and biocides while remaining protected from host immunity. Biofilm can develop within 2–4 days of initial colonisation, and become very tightly attached to extracellular matrix components or the wound bed, making them difficult to remove by surface irrigation or superficial debridement.
Buerger test
Ullamcorper suscipit lobortis nisl ut aliquip ex ea commodo consequat. Duis autem vel eum iriure dolor in hendrerit in vulputate velit esse molestie consequat, vel illum dolore eu feugiat nulla facilisis at vero eros et accumsan et iusto odio dignissim.
Debridement
The European Wound Management Association defines debridement as the “act of removing necrotic material, eschar, devitalized tissue, serocrusts, infected tissue, hyperkeratosis, slough, pus, hematomas, foreign bodies, debris, bone fragments, or any other type of bioburden from a wound with the objective to promote wound healing.
Exudate
Exudate is the fluid that leaks from a wound and is the result of the inflammatory process. Exudate is usually clear or amber coloured and contains proteins, enzymes (especially matrix metallopeptidases /metalloproteinases or MMPs), leucocytes (granulocytes, macrophages), sugar, tissue cells, bacteria, and fungi. While exudate production is a normal feature of healing wounds, over or under production of exudate or exudate of the wrong composition can delay healing. In chronic wounds, exudate slows down or even blocks cell proliferation, interferes with growth factor availability and contains elevated levels of inflammatory mediators and activated MMPs 8-10. Effective exudate management allows moist wound healing and prevents maceration of the wound edge and periwound skin.
Exudate pooling
The accumulation of exudate in the gap between the wound bed and the wound dressing. Exudate pooling is likely in wounds with irregular topographies, pockets, or cavities and this can impact negatively on wound healing by causing maceration and potential infection. Exudate pooling can also occur when the exudate is not absorbed by the wound dressing or the volume of fluid exceeds the dressing’s absorptive capacity. Choosing an appropriate dressing can help manage exudate and reduce the risk of exudate pooling.
Non-healing wounds
Non-healing – has the potential to heal but is not healing due to patient or system factors. For example, a venous leg ulcer is not healing because the patient is unwilling or unable to use compression therapy or compression therapy is not available.
Patient concordance
Also referred to as patient adherence, or patient acceptance, and means how a patient is following the treatment plan. Patient compliance is a term used in the same context, however there is a move away from the term compliance due to its negative connotations.
Periwound skin
Tissue surrounding a wound. Periwound area is traditionally limited to 4cm outside the wound’s edge but can extend beyond this limit if outward damage to the skin is present.
PHMB
Polyhexamethylene Biguanide / Polyhexanide is an active component used to treat local wound infections.
Undermining
Undermining is caused by erosion under the wound edges. Wound undermining occurs when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound’s edge. Undermining is measured by inserting a probe under the wound edge directed almost parallel to the wound surface until resistance is felt.
Undermining with depth or tunneling
Serration of tissue at deeper levels in the wound bed or where the edge of the wound is not attached and a probe will extend into the underlying space.
Vertical absorption
When referring to dressing properties, vertical absorption means the fluid or exudate is taken upward or wicked from the wound bed into the dressing. The dressing then holds the exudate meaning it doesn’t spread laterally or to the sides to leak onto the wound edges or periwound skin. Vertical wicking decreases the chance of maceration of the wound edges and periwound skin.
Wound etiology
Wound etiology refers to the cause of the wound and includes co-morbidities.
Wound progression
Progression, or lack thereof, is improved, unchanged or deteriorated.
